Insurance Training HQ – February 2026 Newsletter
Progress Update, Industry Trends, and What Matters Next
Topics discussed in this Newsletter:
Welcome & February Overview
Training Content & Course Development Update
Job Aids & Reference Materials
Blog Series Update
CMS Final Rule Update
Industry Trends After AEP 2026
Carriers Are Watching More Closely
A Notable Shift: Sales Environment Oversight
Why This Matters Heading Into the Rest of 2026
Looking Ahead & Closing
👋 Welcome & February Overview
February is about momentum.
As we continue building Insurance Training HQ, this month’s newsletter focuses on three things:
Progress on training content and Agent HQ development
What we’re seeing across the Medicare industry post-AEP 2026
Why training and compliance discipline are becoming more critical for agents and agencies moving forward
This newsletter is designed to keep agents informed, help leaders anticipate change, and reinforce why structured training matters now more than ever.
🧩 Training Content & Course Development Update
Where We Are & What’s Coming Next
Our focus remains simple:
Build a foundational Medicare education platform that agents can actually use in real client conversations.
The Medicare Level 100: Core Foundations Series bridges the gap between:
Broad compliance training (AHIP-level)
Product-specific carrier certifications
It gives agents practical, real-world Medicare knowledge — not just surface-level familiarity.
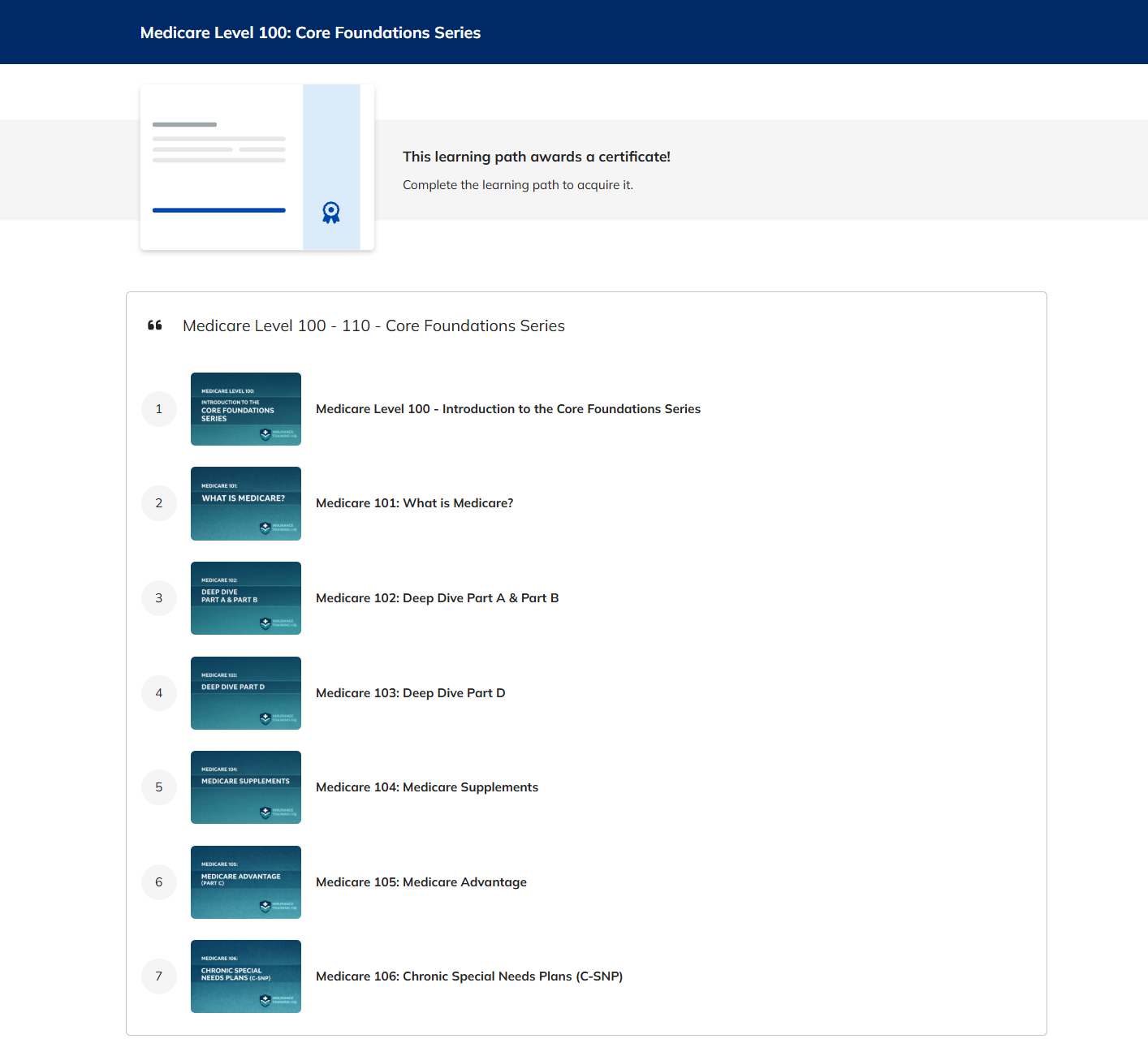
📚Medicare Level 100 Series Progress
Completed:
Medicare 100 through Medicare 106 🎉
Currently in Development:
Medicare 107
Estimated completion: February 18, 2026
Up Next:
Medicare 108 through 110
Estimated full series completion: February 28, 2026
This certification series is designed to help agents:
Build deep Medicare product understanding
Improve plan interaction awareness
Reduce preventable enrollment errors
Strengthen compliance discipline
Increase confidence in client-facing conversations
We will continue sharing updates as we approach full completion of Level 100.
📌 Job Aids & Reference Materials
Supporting Agents at the Moment of Need
Beyond courses, we are building practical tools agents can use between calls, during enrollments, and while preparing for client conversations.
Completed so far:
✅ C-SNP Qualifying Chronic Conditions – Agent Job Aid
Foundational reference for chronic conditions that may qualify under CMS guidelines.
(Used alongside plan verification and eligibility confirmation.)
✅ C-SNP Enrollment & SEP Pathways – High-Level Flow
A visual guide to enrollment pathways and applicable SEPs.
Designed to reduce confusion around C-SNP eligibility and ineligibility timelines.
✅ Medicare Extra Help (LIS) – Agent Job Aid
Clear breakdown of:
LIS levels
What each level covers
Applicable election periods
(SSA makes final eligibility determinations.)
✅ Medicare Savings Program (MSP) – Agent Job Aid
Breakdown of:
Full Medicaid levels
MSP categories
Foundational income/resource awareness
(State rules may vary.)
✅ SPAP vs LIS vs MSP – Key Differences at a Glance
Designed to reduce confusion around assistance programs and election period use.
✅ Medigap – Guarantee Issue Rights by State
Quick reference sheet for state-based GI rights.
📌 These resources will be available inside Agent HQ Plus when the Agent Resource Center launches at the end of Q1.
And more content is coming.
📰 Blog Series Update
Why Training Matters
Over the past month, we’ve published four blog posts focused on:
Onboarding structure
Learning culture
Coaching systems
Retention through development
We will continue this series through the rest of the quarter; next post coming next week!
As we approach SEP selling season, we will gradually shift into:
SEP qualification strategies
Sales positioning tips
Compliance education in real-world context
📜 CMS Final Rule Update
Comment Period Closed—What Happens Next
The public comment period for the proposed CMS Final Rule is now closed.
Key points:
Over 11,000 comments were submitted for CMS review
Comments came from agents, agencies, carriers, advocacy groups, and industry stakeholders
CMS will now review feedback and determine which provisions will move forward, be modified, or be removed
What to Expect Next
CMS typically releases the Final Rule mid-year
Guidance usually comes before AHIP certification
Implementation would apply to Contract Year 2027, impacting AEP 2026–2027
We will break down final decisions once CMS releases official guidance.
📊 Industry Trends After AEP 2026
Post-AEP performance data and regulatory signals continue to reinforce a clear theme:
Quality is winning over volume.
We are seeing a widening gap between:
Agencies with strong training infrastructure
Agencies operating without structured support systems
Leading organizations typically have:
Defined onboarding systems
Ongoing coaching rhythm
Structured compliance oversight
Documented sales standards
Internal accountability frameworks
Others are holding steady, but relying on legacy systems that may not scale under increasing oversight.
Some are faltering, particularly where onboarding and compliance oversight were treated as secondary or reactive functions.
👀 Carriers Are Watching More Closely
Carriers are paying increased attention to:
Complaint Tracking Module (CTM) activity
Rapid disenrollment patterns
Member experience scores
Star Rating performance
Enrollment quality vs volume
Star Ratings directly affect bonus payments and year-round enrollment opportunities.
Carriers have strong incentives to protect quality and reduce preventable complaints.
🔎 A Notable Shift: Sales Environment Oversight
We are observing increased emphasis on controlled sales environments.
More organizations appear to be leaning into:
Field-based agents
Face-to-face enrollment models
Structured appointment settings
Relationship-driven sales approaches
Call center models remain significant, but faster-paced environments require stronger monitoring and coaching systems to maintain compliance stability.
When complaint data becomes more visible and compliance standards tighten:
Oversight becomes strategic.
“Slow and steady” often wins.
In today’s regulatory climate, clean business is a competitive advantage — not just a compliance requirement.
🚨 Why This Matters Heading Into the Rest of 2026
As we move deeper into 2026, the direction is clear:
CMS oversight is increasing
Carriers are tightening standards
Agencies are being held accountable for agent behavior
Agents need better education — not just more pressure
Organizations that invest in structured training, coaching, and support will be better positioned to:
Retain strong agents
Maintain carrier relationships
Reduce compliance exposure
Scale responsibly
This is exactly why Insurance Training HQ exists.
🔭 Looking Ahead & Closing
In the coming months we will:
Complete the Medicare Level 100 Core Foundations Series
Launch the Agent Resource Center
Expand job aids and reference tools
Release SEP selling education
Break down compliance updates in plain language
Thank you for being part of the Insurance Training HQ community.
We’re building with intention.
And we hope you’re building with us.
— Jay Sweat
Founder, Insurance Training HQ
Subscribe to the Newsletter
〰️
Become a Plus Member
〰️
Subscribe to the Newsletter 〰️ Become a Plus Member 〰️
For Agents & Agency Leaders Preparing for What’s Next
Medicare is changing and training matters more than ever—Insurance Training HQ helps you stay informed, prepared, and positioned for what’s coming.
Agent HQ - Light — Free
Includes access to:
Limited free e-learning courses for Aspiring
AgentsMonthly newsletter and industry updates
Agent HQ Plus - $40 / month
Includes access to:
All e-Learning Courses
Full access to training materials, including:
Job aids & Knowledge guides
Short- and long-form video content
Access to new content as it’s released — included in your membership
Monthly newsletter, blog post, and industry updates